Understanding Diabetes: Causes, Types, and Prediabetes Symptoms
- August 23, 2025
- Abrol Hospital
Diabetes is more than just a health condition—it’s a chronic metabolic disorder that affects how your body processes blood sugar (glucose). Glucose is the fuel that keeps us going, but when our body cannot use it properly, things go wrong. Diabetes happens when either the body doesn’t make enough insulin or can’t use it effectively, leading to elevated blood sugar levels.
Understanding diabetes is important because it isn’t just about high sugar levels; if left unchecked, it can damage vital organs like the heart, kidneys, eyes, and nerves. Millions of people worldwide are living with diabetes, and many more are unaware they are in the prediabetic stage. That’s why knowing the causes, signs, and prediabetes symptoms is crucial—it can save lives.
The Basics of Blood Sugar and Insulin
Role of Glucose in the Body
Glucose comes from the food we eat and acts as the main energy source for our cells. Without enough glucose, our body would feel weak and tired. But too much glucose in the bloodstream becomes harmful.
Importance of Insulin
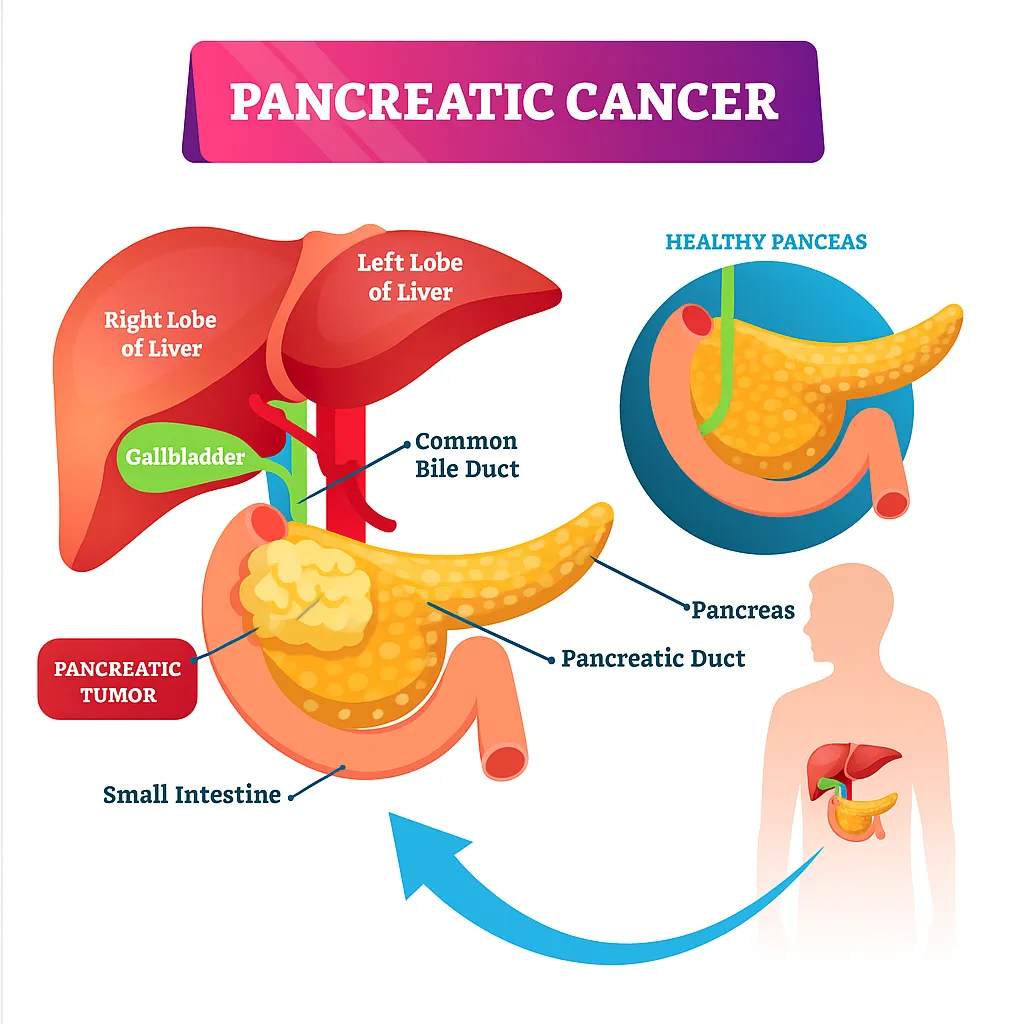
Insulin is a hormone produced by the pancreas. Its role is simple but vital—it helps glucose enter cells to be used as energy. Without insulin, glucose keeps floating in the blood, causing high sugar levels.
What Happens When face High Blood Sugar (Hyperglycemia)
Hyperglycemia is a medical term for high blood sugar. If it happens occasionally, it’s not alarming, but persistent hyperglycemia indicates a serious underlying problem. Over time, it damages blood vessels and organs, leading to diabetes-related complications.
Common Causes of Diabetes
Genetic Factors
Genetics plays a significant role in both type 1 and type 2 diabetes. A family history of diabetes increases the likelihood of developing the condition. In type 1, genetic predisposition can trigger autoimmune responses, while in type 2, inherited insulin resistance tendencies combine with lifestyle factors to cause the disease.
Lifestyle and Dietary Factors
Modern lifestyles characterized by fast food, high sugar intake, and processed diets are strongly linked to diabetes. Excessive consumption of refined carbs and sugary drinks overwhelms the body’s insulin response, leading to insulin resistance.
Obesity and Physical Inactivity
Excess fat, especially around the abdomen, makes it harder for insulin to work effectively. Lack of physical activity further worsens insulin resistance. Together, obesity and inactivity are the biggest modifiable risk factors for type 2 diabetes.
Hormonal and Medical Conditions
Certain conditions, such as PCOS (Polycystic Ovary Syndrome), pancreatitis, or hormonal imbalances, increase diabetes risk. Long-term use of medications like steroids can also impair insulin function.
Different Types of Diabetes
Type 1 Diabetes
Type 1 diabetes is an autoimmune disorder in which the immune system mistakenly attacks insulin-producing cells in the pancreas. As a result, the body cannot produce insulin at all, making insulin therapy essential for survival. It is often diagnosed in childhood or adolescence but can develop at any age.
Type 2 Diabetes
This is the most common type of diabetes, accounting for the majority of cases worldwide. In type 2 diabetes symptoms , the body either resists insulin or does not produce enough of it. Lifestyle factors such as poor diet, obesity, and lack of exercise contribute significantly. Unlike type 1, type 2 can often be managed or even reversed with lifestyle changes if detected early.
Gestational Diabetes
Gestational diabetes occurs in pregnant women when hormonal changes interfere with the body’s ability to use insulin. While it often disappears after childbirth, it increases the risk of developing type 2 diabetes later in life for both the mother and the child. Early diagnosis and careful monitoring are essential to prevent complications.
Other Rare Types
Rare forms include MODY (Maturity Onset Diabetes of the Young), LADA (Latent Autoimmune Diabetes in Adults), and secondary diabetes caused by conditions such as pancreatitis or prolonged steroid use. These types are less common but highlight the complexity of how diabetes can develop.
Understanding Symptoms of Prediabetes
Prediabetes is a stage where blood sugar levels are higher than normal but not high enough to be diagnosed as diabetes. It is often silent, without obvious symptoms, making it easy to miss. Prediabetes is a red flag indicating that your body is struggling with insulin resistance.
Why Prediabetes Should Not Be Ignored
Ignoring prediabetes is dangerous because it significantly increases the risk of developing type 2 diabetes, heart disease, and stroke. Most people with prediabetes progress to diabetes within a decade unless lifestyle changes are made.
Risk Factors for Prediabetes
Factors include being overweight, leading a sedentary lifestyle, poor diet, having a family history of diabetes, and being over 45 years old. Ethnicity also plays a role, with higher risks among Asian, African, and Hispanic populations.
Symptoms of Prediabetes
Subtle Warning Signs: Prediabetes often shows mild symptoms, such as fatigue, slight weight gain, or dark patches on the skin (acanthosis nigricans), particularly around the neck or armpits.
How Prediabetes Differs from Diabetes Symptoms: Unlike diabetes, prediabetes does not cause severe thirst or excessive urination in most cases. Instead, symptoms are subtle, making blood tests crucial for detection.
Long-Term Risks if Ignored: Untreated prediabetes almost always leads to type 2 diabetes. It also increases the risk of cardiovascular disease, kidney problems, and stroke over time.
Managing Diabetes and Prevention of Prediabetes
Lifestyle Changes: Managing diabetes starts with lifestyle changes. These include adopting healthier eating habits, staying active, and reducing stress levels.
Healthy Eating and Balanced Diet: A diet rich in fiber, whole grains, vegetables, lean proteins, and healthy fats helps regulate blood sugar. Processed foods and sugary drinks should be avoided.
Exercise and Physical Activity: Regular physical activity improves insulin sensitivity, lowers blood sugar, and helps maintain a healthy weight. At least 30 minutes of moderate activity daily is recommended.
Medications and Insulin Therapy: In addition to lifestyle changes, medications such as metformin may be prescribed. Type 1 diabetics and some type 2 patients require insulin injections to manage their condition.
Preventing Prediabetes from Progressing
Small Lifestyle Adjustments: Losing just 5–10% of body weight and adding physical activity can dramatically lower the risk of developing diabetes.
Role of Regular Health Checkups: Routine checkups allow early detection and timely management of rising blood sugar levels.
Community and Family Support: Emotional and practical support from family, friends, or support groups can make lifestyle changes easier to maintain.
Related post: Internal Medicine and When Should You See a Specialist
Take Charge of Your Health Today in Gurdaspur – Abrol Hospital
If you or your loved ones are experiencing early signs of diabetes or prediabetes, don’t wait until it progresses further. Consult our experienced Endocrinologist – Diabetes Specialist in Gurdaspur today for accurate diagnosis, personalized care, and long-term health management. Book your appointment now and take the first step towards a healthier future.
FAQs (Frequently Asked Questions)
Common diabetes symptoms include frequent urination, excessive thirst, unexplained weight loss, fatigue, blurred vision, and slow-healing wounds.
Symptoms of high blood sugar include headaches, blurred vision, fatigue, frequent urination, and increased thirst. Severe cases can lead to diabetic ketoacidosis.
To lower blood sugar quickly, drink water, exercise moderately, and follow your doctor’s insulin or medication plan. Always consult a healthcare provider before making changes.
Prediabetes often has no obvious symptoms, but some people may experience fatigue, increased thirst, or darkened skin patches (especially around the neck or armpits).