What Is Pneumonia? Symptoms, Causes, and Treatment
- September 25, 2025
- Abrol Hospital
Pneumonia is a lung infection from bacteria, viruses, or fungi that causes inflammation, breathing difficulty, fever, and other flu-like symptoms. It cause infection that inflames the air sacs in one or both lungs. These air sacs, or alveoli, may fill with fluid or pus, making it difficult to breathe and causing symptoms like coughing, fever, chills, and chest pain. It can range from mild to life-threatening, especially in young children, the elderly, and individuals with weakened immune systems.
Why Is Pneumonia a Serious Health Concern?
Despite being treatable in most cases, pneumonia is still one of the leading causes of death from infectious diseases worldwide. It’s particularly dangerous because it can escalate quickly, leading to severe complications like respiratory failure or even death if not treated promptly.
What’s the Difference Between Viral and Bacterial Pneumonia?
Viral and bacterial pneumonia differ in onset, symptoms, and treatment. Bacterial pneumonia strikes suddenly with high fever and mucus-producing cough, while viral pneumonia develops gradually with dry cough, fatigue, and moderate fever. Diagnosis involves blood tests, sputum cultures, and chest X-rays. Treatment varies—antibiotics for bacterial cases, antivirals and supportive care for viral ones. Recognizing the type is key to effective recovery.
Nature of Fever, Cough, Symptoms
In bacterial pneumonia, fever is typically high, the cough produces thick yellow or green mucus, and the systemic symptoms are more intense.
In viral pneumonia, the fever may be moderate, cough is often dry (or with scant sputum), and symptoms like aches, headaches, and fatigue are more prominent.
What Causes Pneumonia — Types and Agents
Knowing what causes pneumonia helps us tailor both prevention and therapy. Multiple kinds of pathogens can trigger pneumonia:
Bacterial Pneumonia
This is one of the most common pneumonia causes. Common bacterial agents include Streptococcus pneumoniae, Haemophilus influenzae, Staphylococcus aureus, and atypical ones like Mycoplasma pneumoniae. Bacterial pneumonia often leads to more abrupt, aggressive symptoms, and tends to respond well to antibiotics if identified early.
Viral Pneumonia
Viruses such as influenza, respiratory syncytial virus (RSV), adenovirus, and coronaviruses (including SARS‑CoV‑2) are frequent causes of pneumonia. These often precede or predispose to bacterial coinfections.
Fungal Pneumonia
Fungi like Cryptococcus, Histoplasma, Aspergillus, and Pneumocystis jirovecii cause pneumonia mainly in people with severely weakened immunity (e.g. HIV, transplant recipients). The progression can be gradual but serious.
Mycoplasma (Atypical) Pneumonia
Mycoplasma pneumoniae causes a milder, atypical pneumonia often called “walking pneumonia.” Though symptoms are less severe, it can linger. It’s somewhere in between bacterial and viral in behavior.
Mixed & Opportunistic Infections
Especially in immunocompromised individuals, mixed infections (viral + bacterial + fungal) may occur. Opportunistic organisms exploit weakened defenses and cause pneumonia.
Community‑Acquired Pneumonia (CAP)
This is pneumonia acquired outside of healthcare settings. It’s the most common, and its cause spectrum includes typical and atypical bacteria, viruses, and fungi.
Hospital‑Acquired Pneumonia (HAP)
When pneumonia occurs 48 hours or more after hospital admission (and was not incubating at admission), it’s HAP. These are often more resistant to standard antibiotics and associated with more complications.
Ventilator‑Associated Pneumonia (VAP)
A subtype of HAP, VAP develops after mechanical ventilation (often after 48 hours). Intubation gives direct access for pathogens to the lower airway.
Aspiration Pneumonia
This happens when foreign material (food, liquid, vomit) is inhaled into the lungs. Its bacterial mix is often different (more anaerobic bacteria).
These classifications address causes & types of pneumonia by their causative organisms and guide targeted pneumonia treatment.
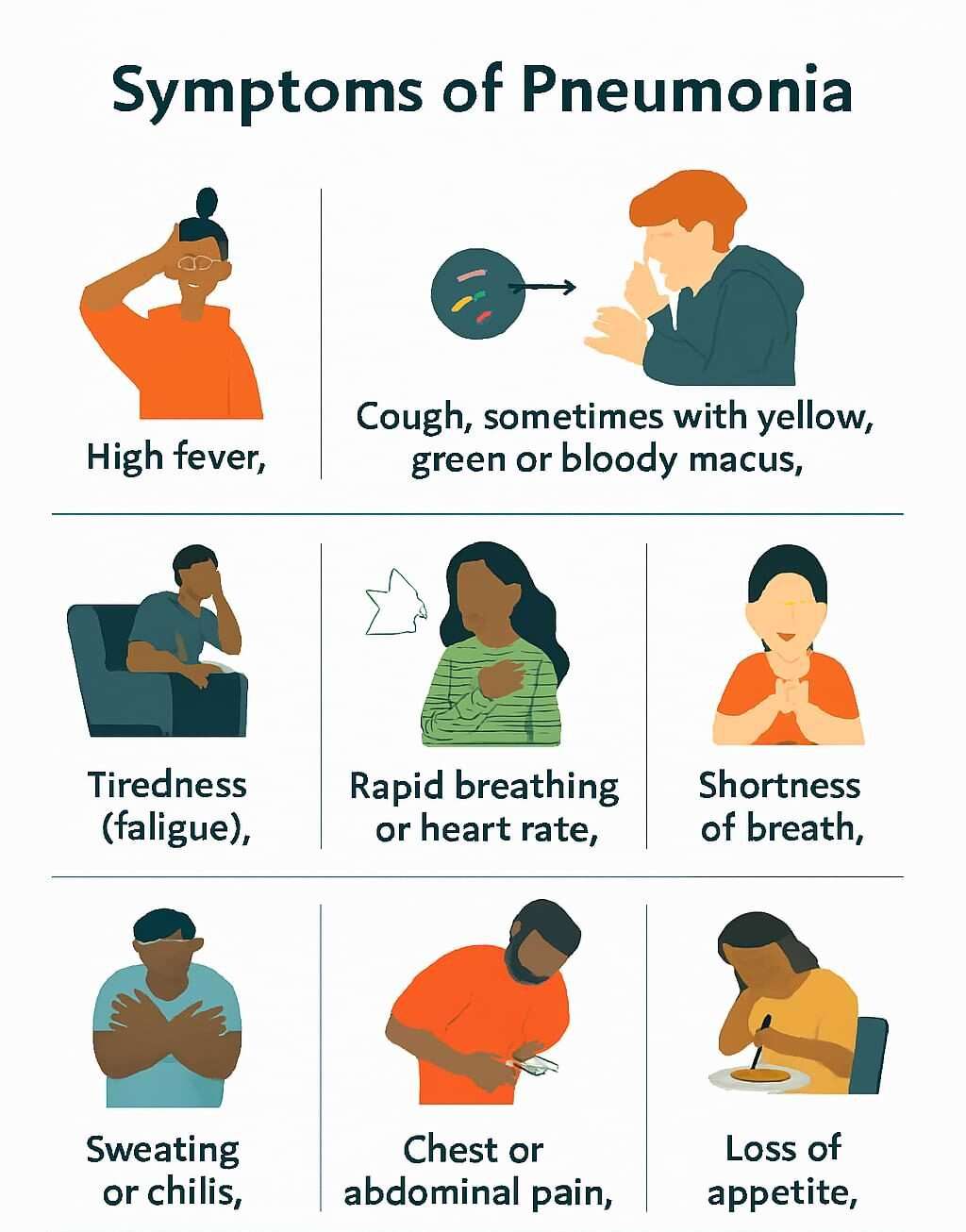
Pneumonia Symptoms — Recognizing the Body Symptoms
Let’s dive into pneumonia symptoms and symptoms of pneumonia, making sure you know when to worry.
Common Pneumonia Symptoms in Adults
Cough: This may start dry and later become productive (with sputum), often green, yellow, or even blood‑tinged.
Fever and chills: Sudden onset high fever, shaking chills, sweats.
Chest pain: Sharp or stabbing pain when breathing deeply or coughing (pleuritic chest pain).
Shortness of breath: Feeling that you cannot catch your breath, especially with minimal exertion.
Fatigue, malaise, muscle aches: A general “hit by a truck” feeling.
Confusion or altered mental status: Especially in older adults.
These are classic pneumonia symptoms and help distinguish it from a simple cold or bronchitis.
Symptoms of Pneumonia in Children and Infants
Irritability, lethargy, or poor feeding (in infants).
Rapid, shallow breathing or grunting.
Chest wall retractions or using accessory muscles of breathing.
Bluish lips (cyanosis) or nail beds in severe cases.
Fever, sometimes very high or sometimes low-grade.
Treatment & Relief Options for Pneumonia
Oxygen Therapy
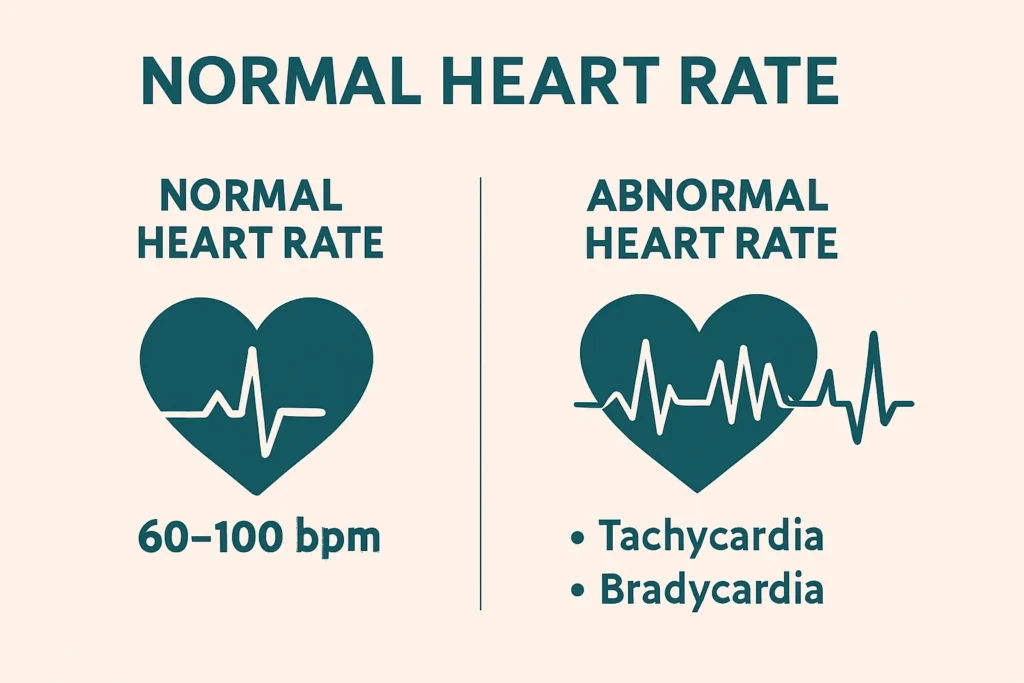
If pneumonia causes shortness of breath or your blood oxygen levels fall below normal, oxygen therapy can offer fast and effective relief. This involves supplying extra oxygen through a nasal cannula, face mask, or mechanical ventilator, depending on severity.
Oxygen therapy helps ensure your organs receive enough oxygen to function properly. It’s commonly used in hospitals for moderate to severe pneumonia but can also be used at home in some chronic cases. Keeping oxygen levels stable is critical for preventing complications like respiratory failure.
Home Remedies & Supportive Care
Supportive care plays a vital role in recovery, especially in cases of mild pneumonia being treated at home. Here are key practices that promote healing:
- Stay well-hydrated: Drinking warm fluids helps loosen mucus in the lungs.
Rest and sleep: Let your body use its energy to fight the infection.
Use a humidifier or steam inhalation: Moist air soothes irritated lungs and helps clear mucus.
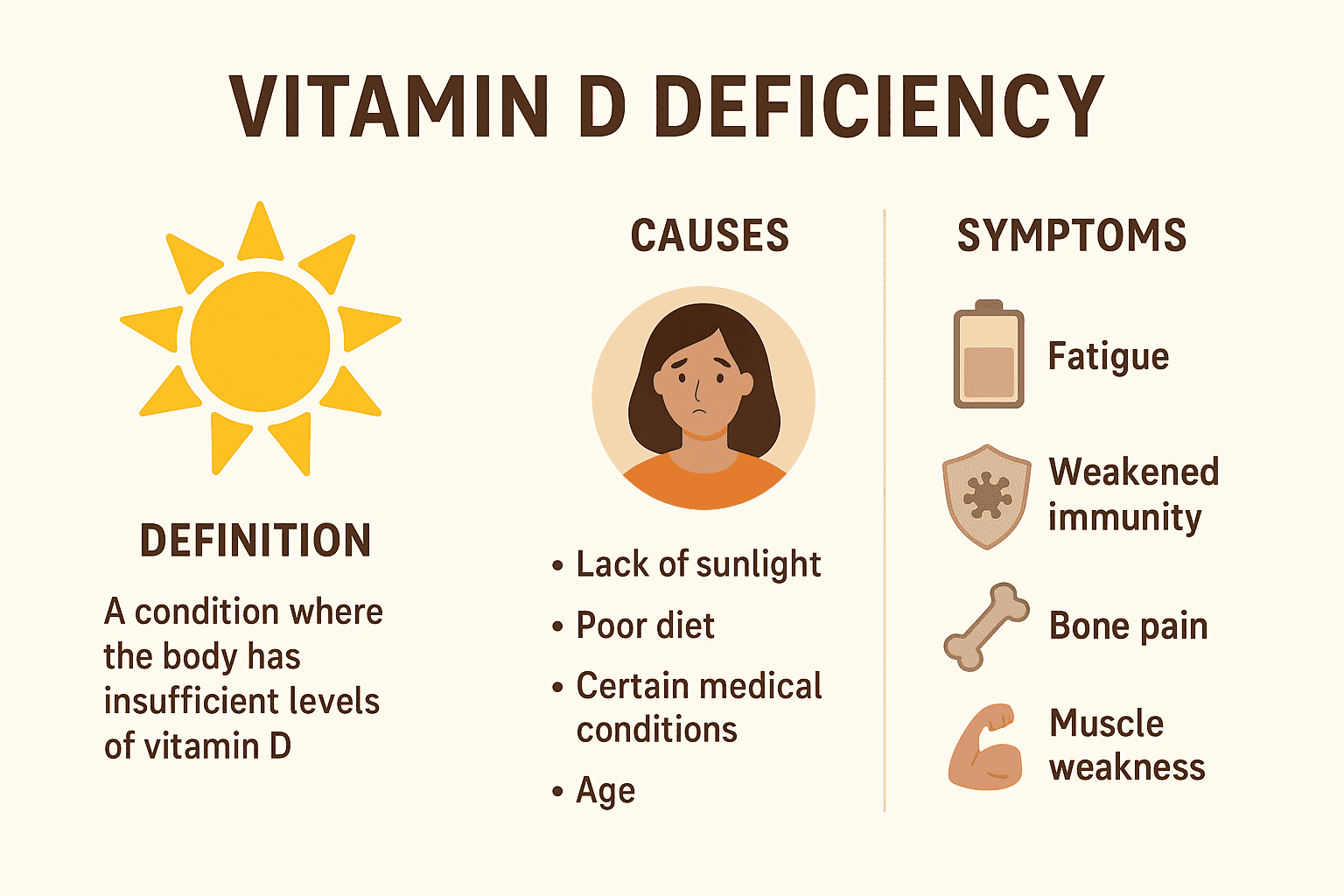
Nutrition: Eating foods rich in vitamin B, A, C, D, and zinc supports the immune system.
Natural remedies like honey and ginger tea can calm sore throats and reduce inflammation.
- Though these aren’t substitutes for medical treatment, they can drastically improve comfort and speed up recovery when used alongside doctor-prescribed medications.
Pulmonary Rehabilitation & Breathing Exercises
After the infection clears, many pneumonia patients experience lingering fatigue, weakness, or shortness of breath. That’s where pulmonary rehab and breathing exercises come in. These treatments aim to rebuild lung strength and improve overall breathing capacity.
Some effective options include:
Incentive spirometry: A handheld device that encourages deep breathing to reopen collapsed air sacs in the lungs.
Pursed-lip breathing: Helps control shortness of breath by slowing down breathing.
Chest physiotherapy: Involves gentle tapping or vibration on the chest to loosen mucus.
🩺 Take Control of Your Health – Consult Expert Doctor for Pneumonia Treatment Today
Neumonia is not just a common cold or seasonal flu—it’s a serious lung infection that demands timely, accurate, and effective medical care. Whether you’re experiencing persistent pneumonia symptoms, have been diagnosed recently, or are still unsure what’s causing your cough, chest pain, or fever, don’t wait for your condition to worsen.
Our highly experienced and compassionate doctors in Gurdaspur, Punjab is here to help you or your loved ones recover safely and quickly from pneumonia—be it bacterial, viral, or fungal in nature.
Why Choose Us?
• Expert Diagnosis & Tailored Treatment Plans
• Full guidance on pneumonia symptoms, cause, and types
• Access to advanced care including antibiotics, antivirals, oxygen therapy, and home-care advice
• Support for all age groups – from children to elderly
FAQs (Frequently Asked Questions)
Recovery from pneumonia typically takes 1 to 3 weeks for mild cases, but more serious cases can take up to 6 to 8 weeks or longer—especially in older adults, smokers, or those with underlying health conditions. The duration depends on the type of pneumonia, the patient’s overall health, and how quickly treatment began. Rest, hydration, and following your prescribed pneumonia treatment plan are essential for a full recovery.
The main cause of pneumonia is an infection that inflames the air sacs in one or both lungs. This infection can be caused by:
Bacteria (most common)
Viruses (like influenza or COVID-19)
Fungi (in people with weakened immune systems)
Among bacterial causes, Streptococcus pneumoniae is the most common culprit. Identifying what causes pneumonia helps doctors provide the right treatment, whether it’s antibiotics, antivirals, or antifungals.
Yes, certain types of pneumonia, especially viral and bacterial pneumonia, can be contagious. You can catch pneumonia through:
Coughing or sneezing (airborne droplets)
Touching contaminated surfaces
Close contact with an infected person
However, not everyone who is exposed will develop pneumonia. It depends on your immune system, age, and existing health conditions. Good hygiene and vaccinations can help prevent catching pneumonia.