Pancreatic Cancer: Causes, Symptoms, and Treatment Options
- August 11, 2025
- Abrol Hospital
Pancreatic cancer is one of the most serious and life-threatening cancers because of its silent progression and rapid spread. Located deep in the abdomen, the pancreas is a vital organ that quietly performs crucial tasks for digestion and blood sugar regulation. Unfortunately, its hidden position often allows tumors to grow unnoticed until they reach advanced stages or diagnose by abdominal ultrasound. This is why pancreatic cancer is often referred to as a “silent killer.” Early diagnosis can dramatically improve treatment success rates, but in reality, most cases are diagnosed late. Raising awareness about its causes, symptoms, and treatments can help change that.
What is Pancreatic Cancer?
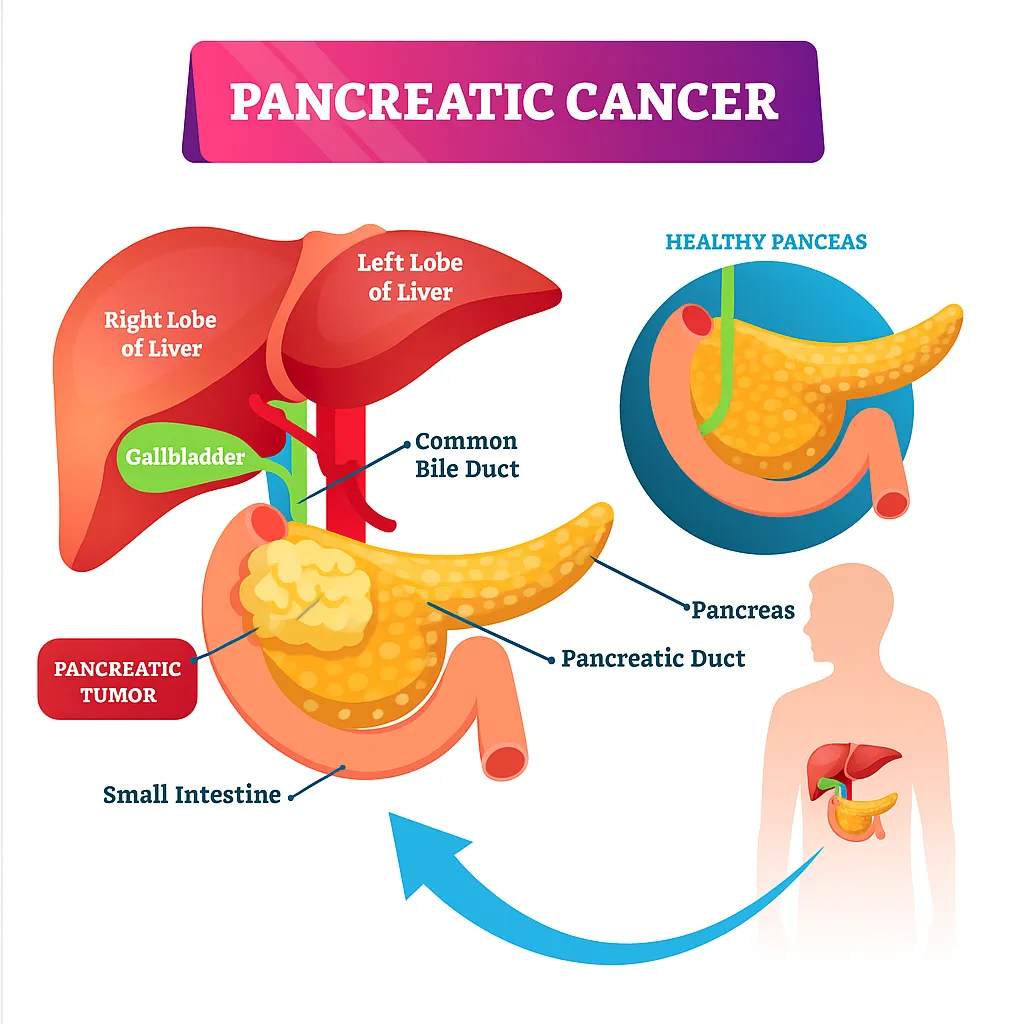
Pancreatic cancer develops when abnormal cells in the pancreas start to multiply uncontrollably, forming malignant tumors. These cancerous cells disrupt the pancreas’s normal function and can spread to other parts of the body. There are two main types:
Exocrine tumors, which make up the majority of cases and affect the enzyme-producing cells.
Endocrine tumors, which are less common and affect hormone-producing cells.
The most common type, pancreatic adenocarcinoma, is especially aggressive and begins in the pancreatic ducts.
Importance of Early Detection
Detecting pancreatic cancer early is challenging because initial symptoms are either mild or mistaken for other conditions. However, catching it early can mean the difference between life-saving surgery and only palliative care. Early detection allows for more treatment options, including surgical removal of the tumor, which can potentially cure the disease. That’s why understanding the warning signs and risk factors is so vital.
Understanding the Pancreas & Its Role in the Body
In order to ensure that the body absorbs nutrients effectively, it creates digestive enzymes that aid in the breakdown of fats, proteins, and carbs which helps to improve your digestive system. Additionally, it releases chemicals that regulate blood sugar levels, such as glucagon and insulin. Without a functioning pancreas, both digestion and metabolism would be severely impaired.
How Cancer Affects Pancreatic Function
When cancer develops, it can block the release of digestive enzymes, leading to malnutrition and weight loss. Tumors can also interfere with hormone production, causing sudden-onset diabetes in some patients. As the tumor grows, it can press on nearby organs and nerves, causing pain and other complications.
Causes of Pancreatic Cancer
Genetic Mutations
DNA damage within pancreatic cells can cause them to grow out of control. Mutations in genes such as BRCA1, BRCA2, and p53 are linked to higher pancreatic cancer risk. While some mutations evolve over time as a result of environmental and lifestyle factors, others are inherited.
Lifestyle-Related Risk Factors
Smoking, heavy alcohol use, and diets high in saturated fat can increase the risk. Cigarette smoke contains carcinogens that can directly damage pancreatic cells, while alcohol abuse can trigger chronic inflammation of the pancreas.
Medical Conditions Increasing Risk
Diseases like chronic pancreatitis, long-standing diabetes, and certain infections have been shown to raise the likelihood of pancreatic cancer. Chronic pancreatitis, in particular, creates an environment of continuous cell damage and repair, which can eventually lead to mutations.
Family History and Hereditary Syndromes
A family history of pancreatic cancer or certain hereditary syndromes (like Lynch syndrome) significantly raises risk. People with multiple relatives affected should consider genetic testing.
Risk Factors You Should Know
Age and Gender
The risk of developing pancreatic cancer rises sharply after age 60. Men are slightly more prone than women, possibly due to higher rates of smoking and occupational exposures.
Smoking and Alcohol Consumption
Smoking nearly doubles the risk of pancreatic cancer. Alcohol, especially in large quantities, can damage the pancreas and cause chronic pancreatitis, another risk factor.
Diet and Obesity
Diets rich in red meat, processed foods, and sugary drinks increase inflammation and insulin resistance, both of which can promote cancer growth. Being overweight also places extra stress on the pancreas.
Chronic Pancreatitis
Over time, chronic inflammation weakens pancreatic tissue, which fosters the growth of cancer cells.
Symptoms of Pancreatic Cancer
Early-Stage Symptoms
Early symptoms, like moderate stomach pain, inexplicable exhaustion, and slight weight loss, are frequently ambiguous. Unfortunately, these signs are easily overlooked or attributed to less serious conditions.
Advanced-Stage Symptoms
In later stages, symptoms become more obvious and severe. Jaundice (yellowing of the skin and eyes) occurs when the tumor blocks the bile duct. Patients may also experience dark urine, pale stools, and severe abdominal or back pain.
Symptoms Often Misdiagnosed
Because early signs resemble gallbladder disease, hepatitis, or stomach ulcers, diagnosis is often delayed until the disease is advanced.
Diagnosis & Stages of Pancreatic Cancer
Imaging Tests
CT scans, MRI, and endoscopic/ abdominal ultrasound are the primary tools for detecting pancreatic tumors. These provide detailed images to locate and assess the tumor’s size and spread.
Blood Tests and Tumor Markers
The CA 19-9 blood test measures a protein that may be elevated in pancreatic cancer patients. While not perfect, it can help monitor treatment effectiveness.
Biopsy and Histological Analysis
A biopsy involves removing a small tissue sample from the pancreas for microscopic examination. This confirms whether the tumor is cancerous.
Stages of Pancreatic Cancer
Stage 0 – Carcinoma in Situ
Cancer is confined to the inner lining of the pancreas and has not spread. This stage has the highest cure potential if detected.
Stage I to IV Overview
Stage I: Localized tumor within the pancreas.
Stage II: The tumor has extended to lymph nodes or adjacent tissues.
Stage III: Major blood arteries close to the pancreas have been affected by the cancer.
Stage IV: The liver or lungs are among the distant organs where the cancer has progressed.
How Staging Affects Treatment Choices
Lower stages are often treated with surgery and may be curable, while advanced stages focus on slowing progression and relieving symptoms.
Book a Consultation with Our Doctor Today
Our experienced doctors specialize in Gastrorentrology and oncological care, using advanced diagnostic tools and personalized treatment plans to give you the best possible outcome. From early screening for high-risk individuals to comprehensive treatment strategies, we are committed to providing compassionate, expert care at every stage.
Remember: The difference between a timely check-up and delayed diagnosis could be life-changing.
📞Scedule your consultation and take the first step toward clarity and peace of mind. Your health is worth it — and we’re here to fight alongside you.
FAQs (Frequently Asked Questions)
Many patients report initial symptoms like persistent indigestion, mild abdominal discomfort, fatigue, or unexpected weight loss. However, symptoms can vary greatly between individuals.
Pancreatic cancer is often found through imaging tests like CT scans, MRIs, and endoscopic ultrasounds. Blood tests such as CA 19-9 can provide clues but aren’t definitive. In most cases, a biopsy is performed to confirm diagnosis.
Common symptoms include jaundice (yellowing of the skin and eyes), unexplained weight loss, abdominal or back pain, loss of appetite, nausea, and light-colored stools. In some cases, new-onset diabetes can also be a sign.
Exocrine tumors, the most common type, affect enzyme-producing cells and are usually more aggressive. Endocrine tumors are rarer, affecting hormone-producing cells, and often have a slower growth rate.
The survival rate depends on the stage at diagnosis. Early-stage pancreatic cancer has a higher survival rate, but overall, the 5-year survival rate remains lower than many other cancers due to late detection.
While the exact cause isn’t always clear, risk factors include smoking, chronic pancreatitis, obesity, family history, certain genetic mutations (like BRCA2), and a diet high in processed meats.